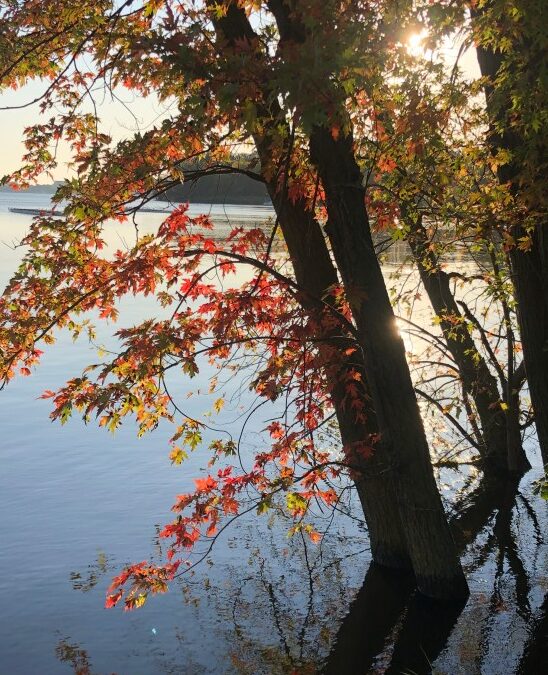
by Jeremy Topin | Oct 28, 2019 | Balance, Family, Parenting, Transformation
The simplest questions/ are the most profound./ Where were you born? Where is your home?/ Where are you going?/ What are you doing?/ Think about these/ once in a while, and/ watch your answers/ change.” Richard Bach: Illusions, The Adventures of a Reluctant Messiah...
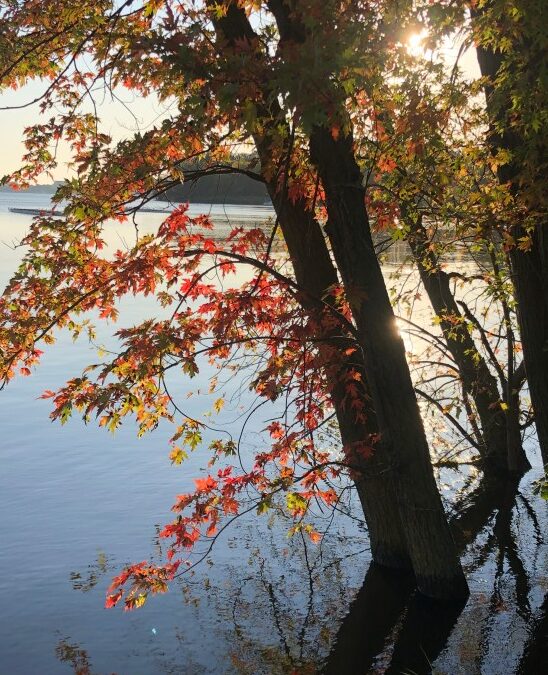
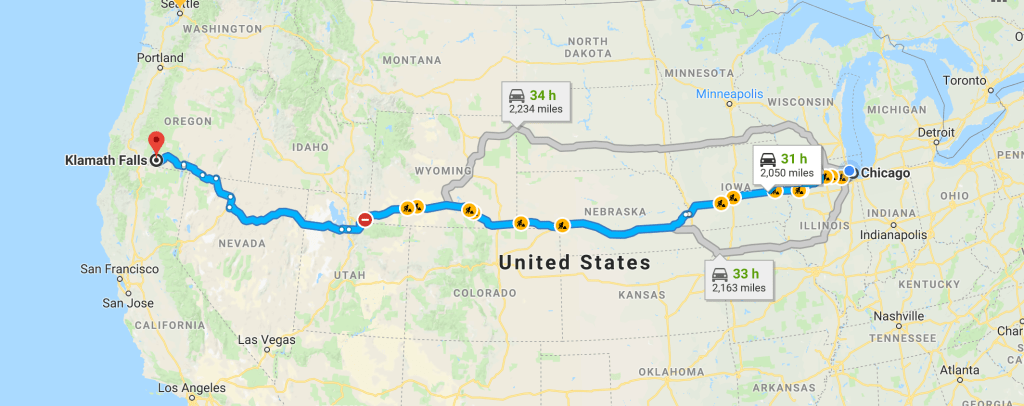
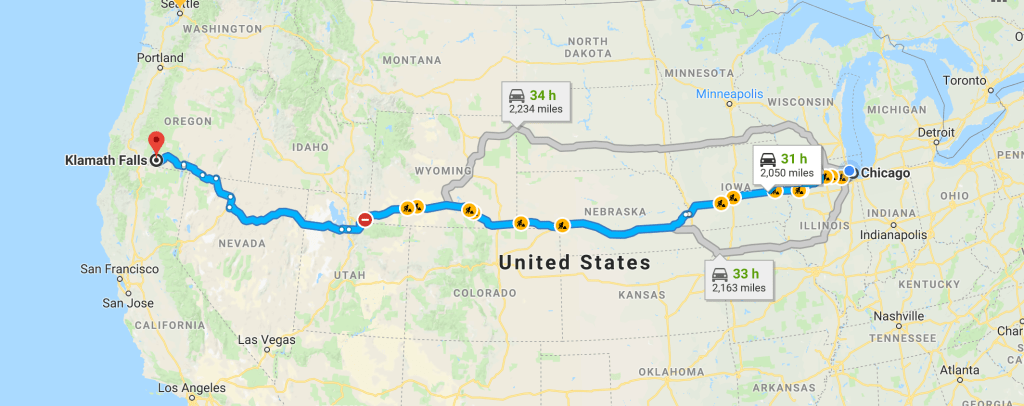
by Jeremy Topin | Apr 8, 2019 | Balance, Family, Parenting, Teenager, Transformation
What would you do for love? That question is often posed during the dizzying intoxication of a new relationship. Answered in romantic comedies by driving cross country or hopping on some transcontinental flight, chasing down one’s true soulmate. It might mean moving...
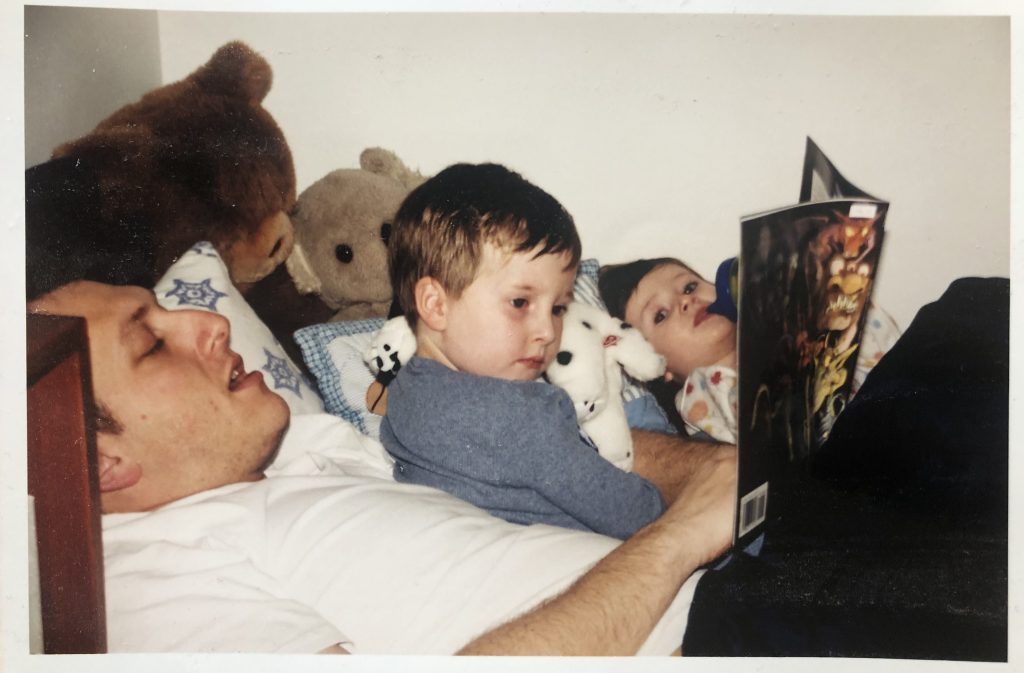
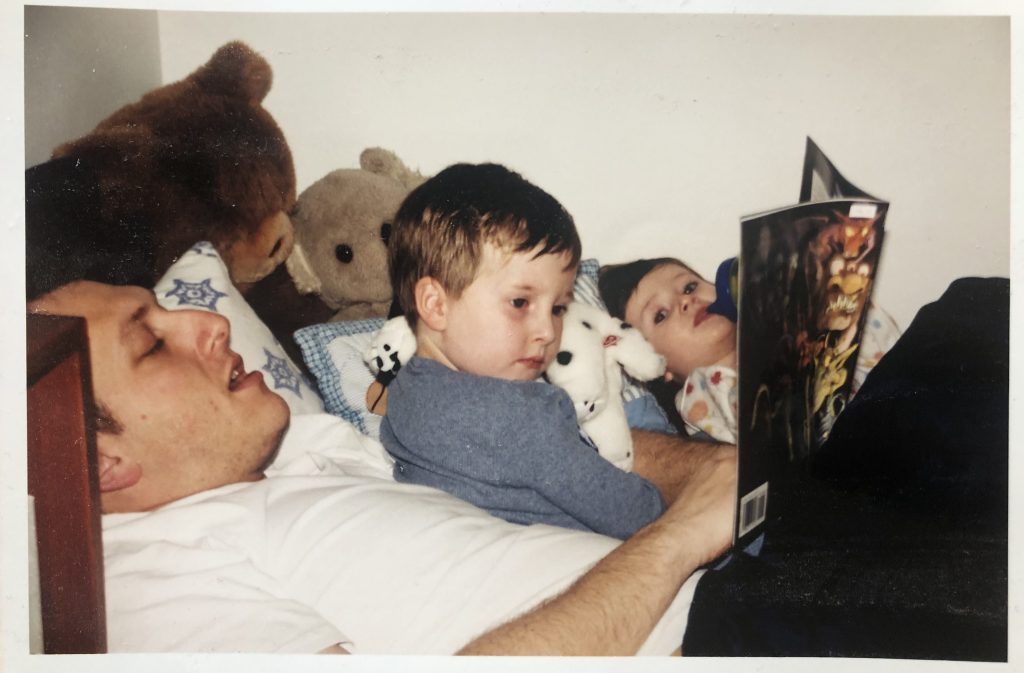
by Jeremy Topin | Nov 22, 2018 | Balance, Family, Parenting, Transformation
For me, holidays such as Thanksgiving, evoke memories more than emotions. Reflection on traditions more than generating a visceral response. The ritual of a 4am wake up alarm followed by a moonlit drive on barren roads to an empty hospital parking lot has been...

by Jeremy Topin | Nov 20, 2018 | Balance, Burnout, Medicine, Parenting, Transformation
This piece recently was published at Doximity’s Op-(m)ed. I worked on this essay for quite a while for publication elsewhere. It does touch on many of the same themes I have already written about on this blog. In that sense, it is not particularly revealing of...

by Jeremy Topin | Oct 26, 2018 | Balance, Change, Transformation
I am excited to bring another guest post to Balance, written by Doctor Monisha Vasa! Monisha is a psychiatrist, mother and writer, currently living in Orange County, California, but has strong ties to Chicago growing up in the southwest suburbs. I have had the...
by Jeremy Topin | Oct 17, 2018 | Balance, Burnout, Change, Medical Education, Mental Health, Parenting, Transformation
I wanted to share a sincere thank you to Elizabeth Metraux at Primary Care Progress, for the opportunity to be interviewed on her Podcast, Relational Rounds. Becky and I were able to share our story from medical school and residency training to fellowship and private...