by Jeremy Topin | Oct 17, 2018 | Balance, Burnout, Change, Medical Education, Mental Health, Parenting, Transformation
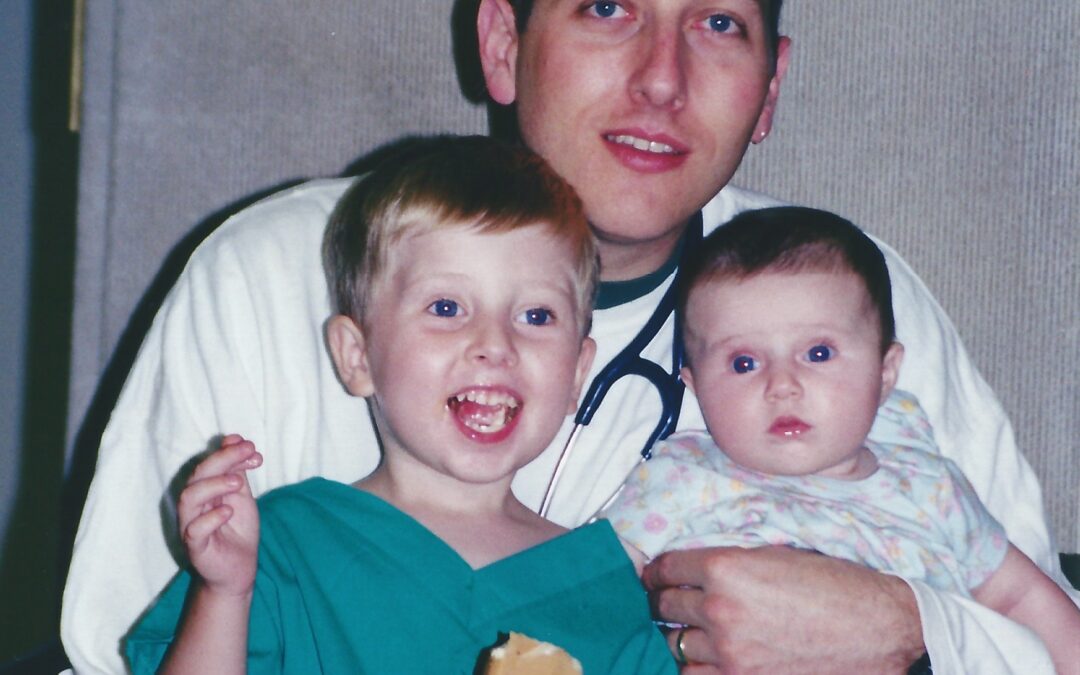
I wanted to share a sincere thank you to Elizabeth Metraux at Primary Care Progress, for the opportunity to be interviewed on her Podcast, Relational Rounds. Becky and I were able to share our story from medical school and residency training to fellowship and private...

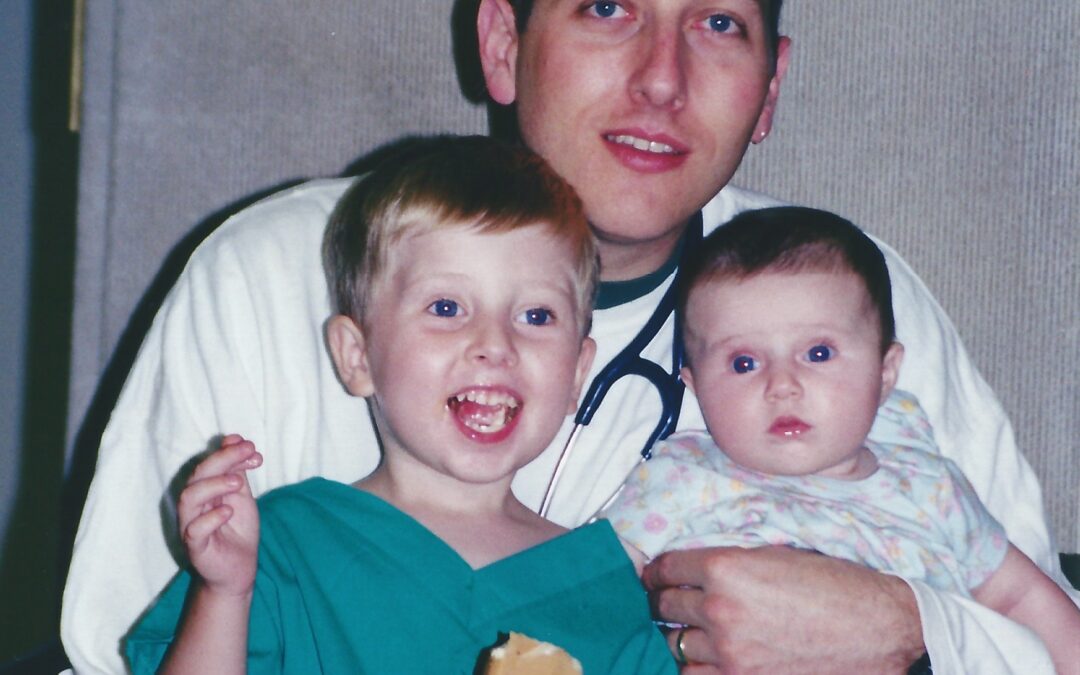
by Jeremy Topin | Aug 28, 2018 | Balance, End of life, Medical, Medical Education, Parenting
It is my pleasure to introduce to the readers of Balance, Dr. Rebecca MacDonell-Yilmaz. Becky is a pediatrician out on the East coast who has not only just completed a fellowship in hospice and palliative care medicine, but has just embarked on her third board...

by Jeremy Topin | Jun 2, 2018 | Change, Medical Education
Welcome new PG-1’s! One day you wake up a medical student. Then by the afternoon you are a MD. A few short days later, you are now in the hospital no longer looking for someone to co-sign your orders in the EMR. It’s a crazy time, full of excitement as well as an...

by Jeremy Topin | May 3, 2018 | Double Effect, End of life, Medical Education, Medicine, Palliative Care
This post was first published on Doximity’s Op-(M)ed “First Stab” Collection on 5/2/18 under the title: Should I Heal or Comfort? Chicago, in February, was dark and cold. Even more so at 5:00 AM, when scraping ice and snow from my windshield before...
by Jeremy Topin | Oct 17, 2017 | Balance, Burnout, Healthcare Reform, Medical Education, Medicine, Parenting
The day began the same as yesterday. As well as every day prior to that for the last few months. I was tired. Exhausted. The type of fatigue that envelops your brain in a dense fog, altering the way you see and hear the world around you. The type that impairs your...

by Jeremy Topin | Aug 18, 2017 | End of life, Medical Education, Medicine
“Doctor…She wants a chance. She wants to live!” How often have I heard those words? Or some version of them? The location of the conversations varies. I might be standing outside the curtain of an emergency room bay or sitting on a worn chair inside a cramped waiting...