by Jeremy Topin | Apr 8, 2019 | Balance, Family, Parenting, Teenager, Transformation
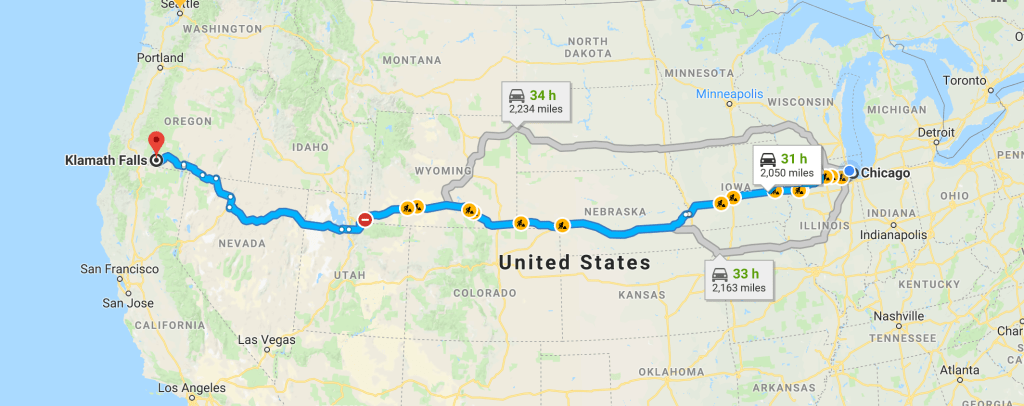
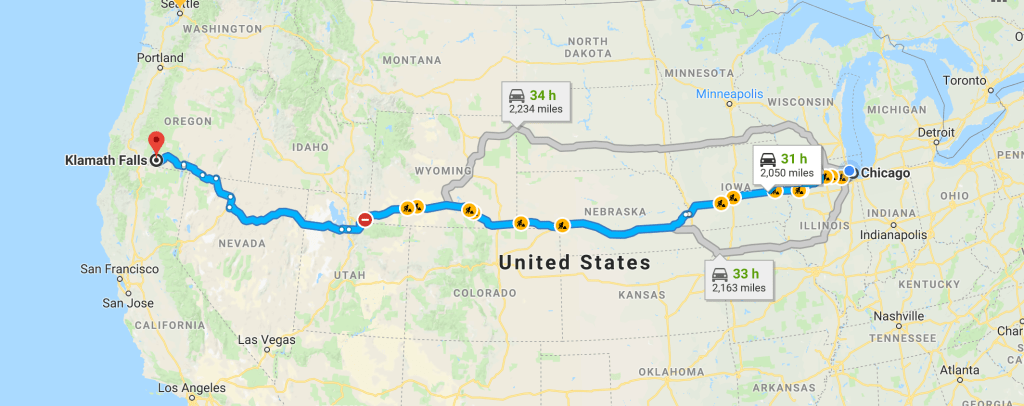
What would you do for love? That question is often posed during the dizzying intoxication of a new relationship. Answered in romantic comedies by driving cross country or hopping on some transcontinental flight, chasing down one’s true soulmate. It might mean moving...

by Jeremy Topin | Dec 11, 2018 | Burnout, Change, Family, Parenting, Teenager
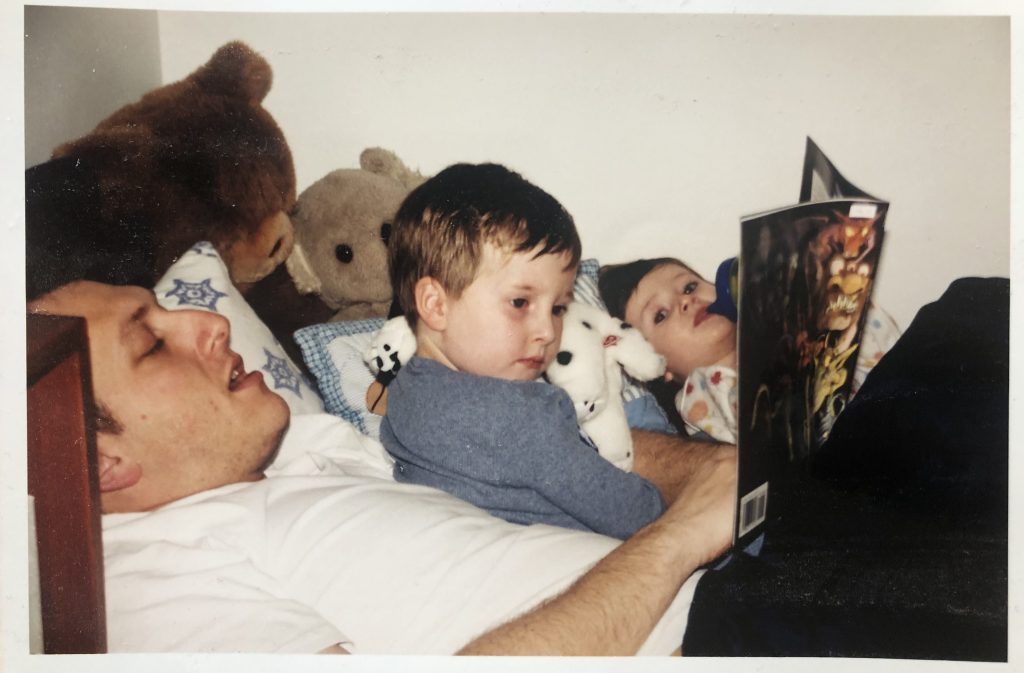
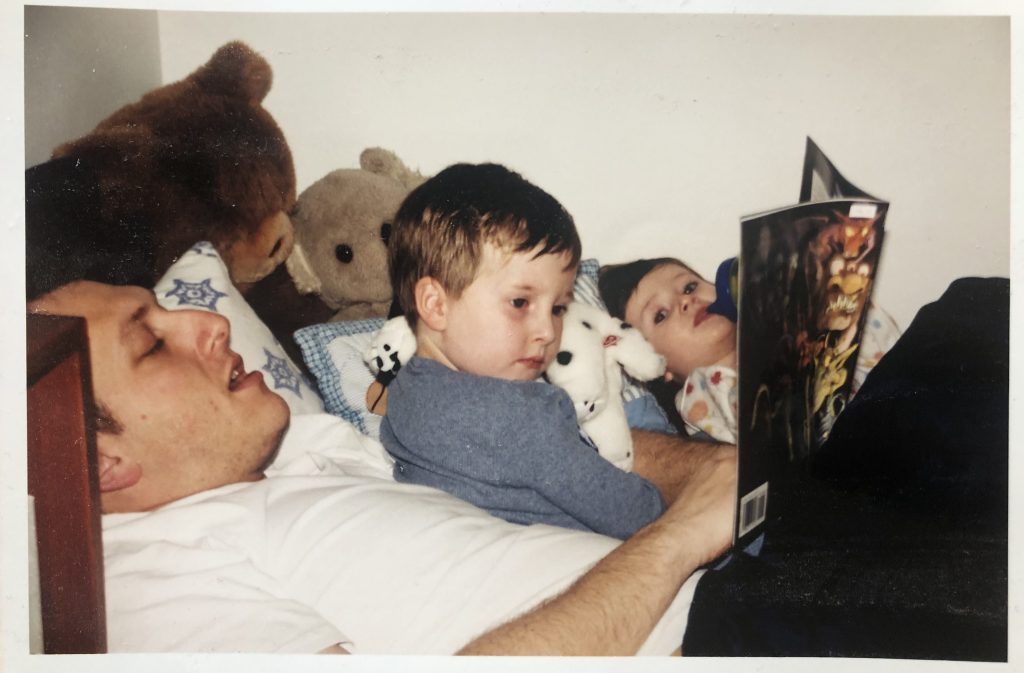
I miss when you both were little. The three of us with room to spare in the big chair. That precious time before you would sleep, wearing soft PJ’s dotted in animal shapes. I preferred the ones without “footsies”, so I could feel those small, cold feet brush against...
by Jeremy Topin | Nov 22, 2018 | Balance, Family, Parenting, Transformation
For me, holidays such as Thanksgiving, evoke memories more than emotions. Reflection on traditions more than generating a visceral response. The ritual of a 4am wake up alarm followed by a moonlit drive on barren roads to an empty hospital parking lot has been...
by Jeremy Topin | Oct 17, 2018 | Balance, Burnout, Change, Medical Education, Mental Health, Parenting, Transformation
I wanted to share a sincere thank you to Elizabeth Metraux at Primary Care Progress, for the opportunity to be interviewed on her Podcast, Relational Rounds. Becky and I were able to share our story from medical school and residency training to fellowship and private...

by Jeremy Topin | Aug 28, 2018 | Balance, End of life, Medical, Medical Education, Parenting
It is my pleasure to introduce to the readers of Balance, Dr. Rebecca MacDonell-Yilmaz. Becky is a pediatrician out on the East coast who has not only just completed a fellowship in hospice and palliative care medicine, but has just embarked on her third board...