by Jeremy Topin | Oct 28, 2019 | Balance, Family, Parenting, Transformation
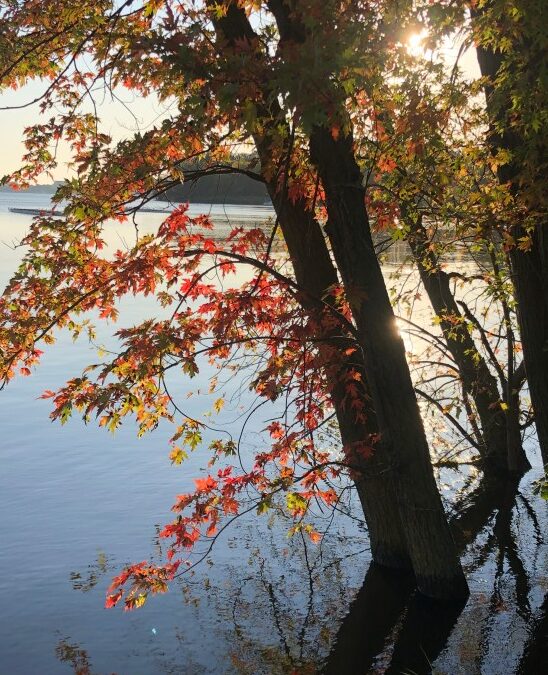
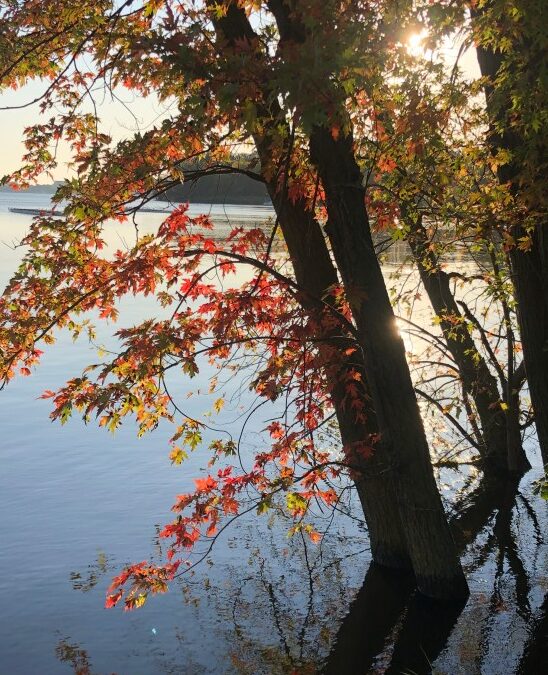
The simplest questions/ are the most profound./ Where were you born? Where is your home?/ Where are you going?/ What are you doing?/ Think about these/ once in a while, and/ watch your answers/ change.” Richard Bach: Illusions, The Adventures of a Reluctant Messiah...

by Jeremy Topin | Jun 12, 2019 | Burnout, Family, Parenting, Teenager, Transformation
Maya, As I sit in the balcony watching, your distinct smile is visible from afar. You and 500 other students are about to receive your diplomas and, in the process, cross over from high school students to graduates. Our house has been hectic this past week with all...
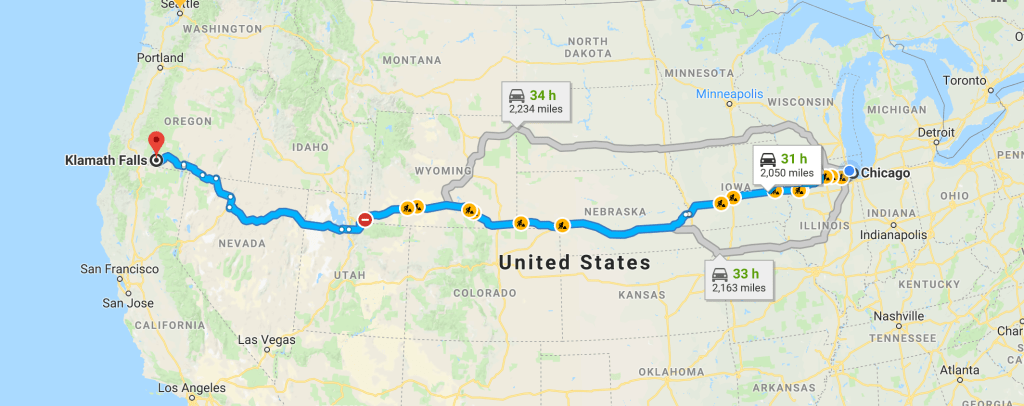
by Jeremy Topin | Apr 8, 2019 | Balance, Family, Parenting, Teenager, Transformation
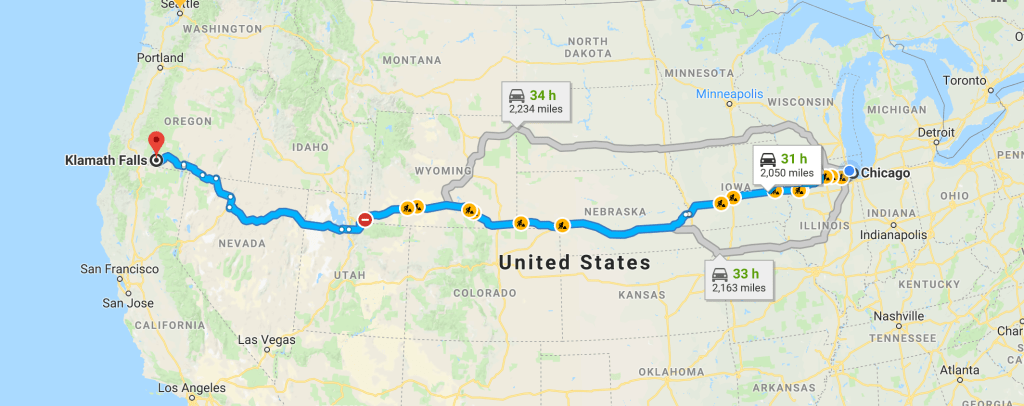
What would you do for love? That question is often posed during the dizzying intoxication of a new relationship. Answered in romantic comedies by driving cross country or hopping on some transcontinental flight, chasing down one’s true soulmate. It might mean moving...

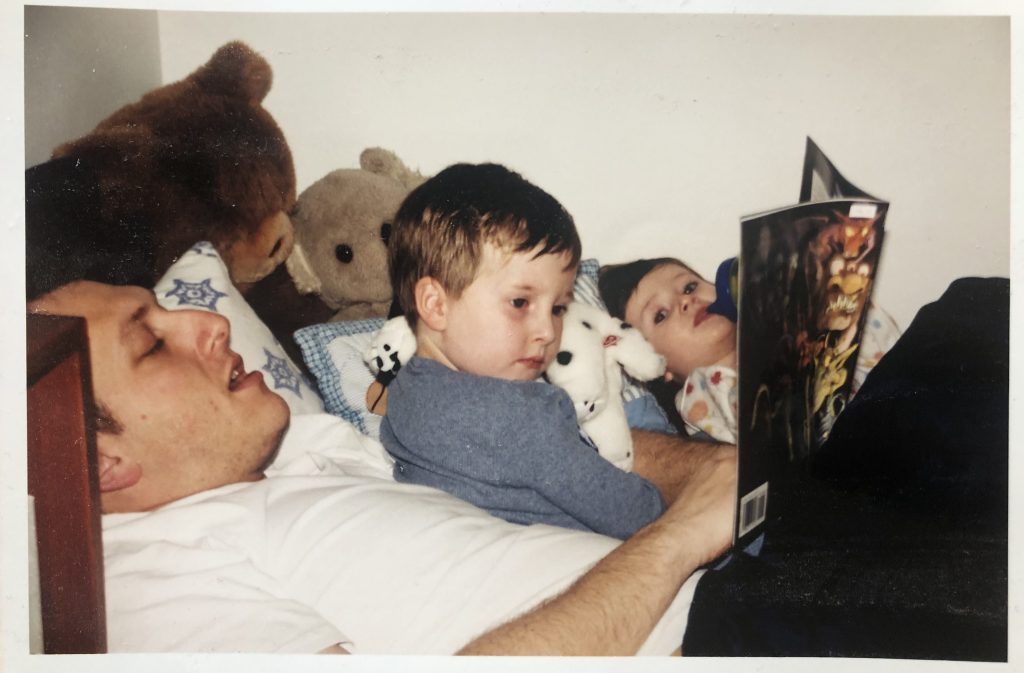
by Jeremy Topin | Dec 11, 2018 | Burnout, Change, Family, Parenting, Teenager
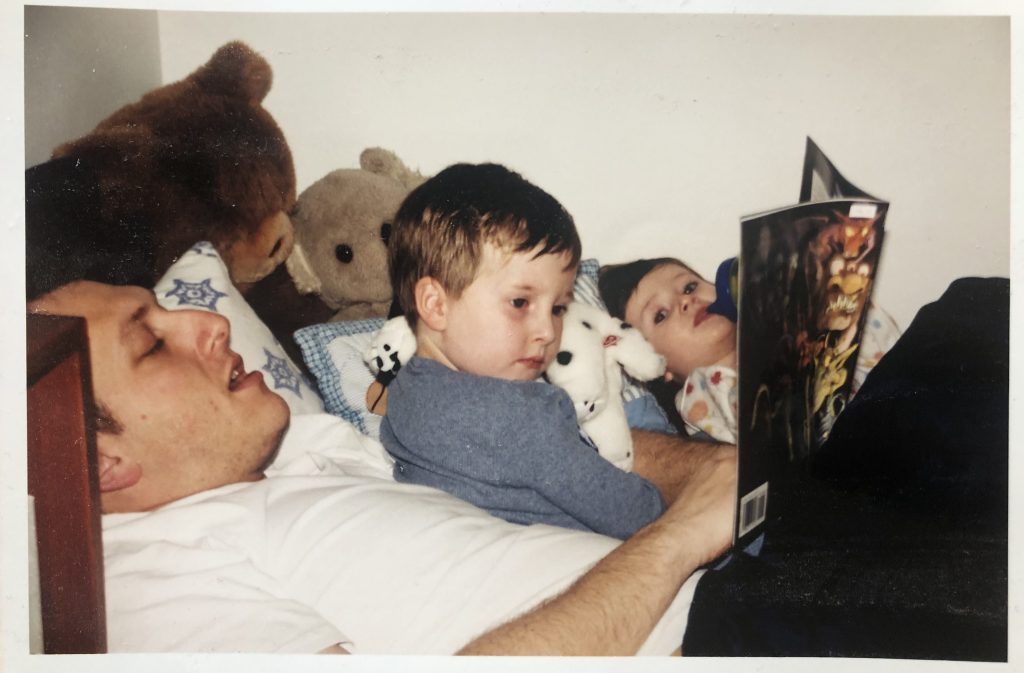
I miss when you both were little. The three of us with room to spare in the big chair. That precious time before you would sleep, wearing soft PJ’s dotted in animal shapes. I preferred the ones without “footsies”, so I could feel those small, cold feet brush against...
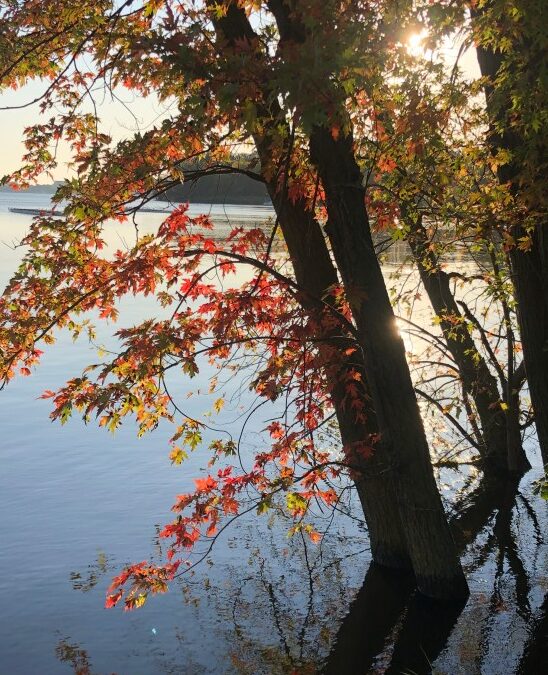
by Jeremy Topin | Nov 22, 2018 | Balance, Family, Parenting, Transformation
For me, holidays such as Thanksgiving, evoke memories more than emotions. Reflection on traditions more than generating a visceral response. The ritual of a 4am wake up alarm followed by a moonlit drive on barren roads to an empty hospital parking lot has been...

by Jeremy Topin | Nov 20, 2018 | Balance, Burnout, Medicine, Parenting, Transformation
This piece recently was published at Doximity’s Op-(m)ed. I worked on this essay for quite a while for publication elsewhere. It does touch on many of the same themes I have already written about on this blog. In that sense, it is not particularly revealing of...