by Jeremy Topin | Oct 17, 2018 | Balance, Burnout, Change, Medical Education, Mental Health, Parenting, Transformation
I wanted to share a sincere thank you to Elizabeth Metraux at Primary Care Progress, for the opportunity to be interviewed on her Podcast, Relational Rounds. Becky and I were able to share our story from medical school and residency training to fellowship and private...

by Jeremy Topin | Aug 28, 2018 | Balance, End of life, Medical, Medical Education, Parenting
It is my pleasure to introduce to the readers of Balance, Dr. Rebecca MacDonell-Yilmaz. Becky is a pediatrician out on the East coast who has not only just completed a fellowship in hospice and palliative care medicine, but has just embarked on her third board...

by Jeremy Topin | Aug 22, 2018 | Balance, Change, Parenting, Transformation
I am sitting in the parking lot, waiting for the local bookstore, The Book Bin, to open. I am here because of a flower. And a pear tree turned maple. And a sense of time and space. And the writer Dostoyevsky. Sipping my morning coffee, with the Jeep’s soft top down, I...

by Jeremy Topin | Aug 9, 2018 | Balance, Parenting, Teenager, Transformation, Triathlon
Two friends (younger than me by more than two decades) are training for the Ironman and I decided to join them for their first of two 40-mile loops. I had already decided to defer my own race entry to next year due to a combination of aches and pains, along with...

by Jeremy Topin | Aug 7, 2018 | Balance, Parenting, Uncategorized
Picture Credit (John Moore/Getty Images) “…if we forget, we are guilty, we are accomplices. “we must always take sides. Neutrality helps the oppressor, never the victim. Silence encourages the tormentor, never the tormented. Sometimes we must...
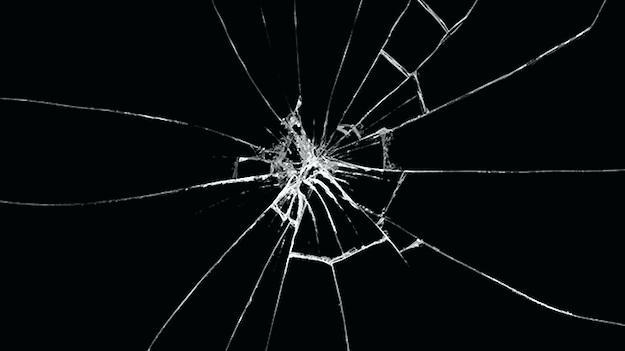
by Jeremy Topin | Apr 20, 2018 | Balance, Burnout, Change, Healthcare Reform, Medicine, Parenting, Transformation
How do you know when someone is broken? When their spirit is fractured? When their sense of self no longer aligns with what once was. When you feel as if you have woken up in a foreign land, but that sense of displacement is coming from you, not your surroundings. In...